50 years after Bright
Richard Bright’s 1827 report created the discipline of nephrology and triggered an exciting period of clinical research into kidney disease.
William Howship Dickinson (1832-1913) was one of these early nephrologists, employed at Great Ormond St Children’s Hospital in London. In addition to an interest in neurology he wrote a notable three-part series Diseases of the Kidney and Urinary Derangements between 1865 and 85.
Most of his cases of acute nephritis (‘tubal and diffuse nephritis’) were what we would now call post-Streptococcal glomerulonephritis.
The condition had long been recognised, but its nature was becoming much better understood. Pierre Rayer in Paris played a major part by identifying the association of this variant of Bright’s disease with haematuria. Its causes were believed to be:
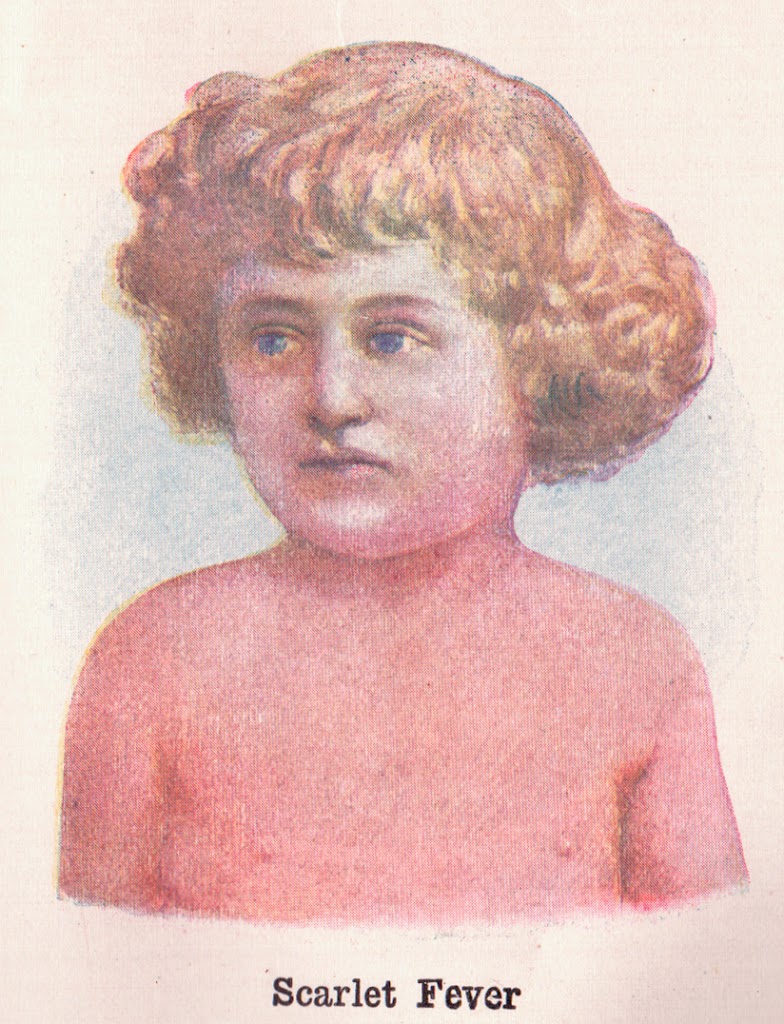
- Scarlatina (scarlet fever, Fig 1) – i.e. a consequence of Streptococcal infection. The association of scarlatina with nephritis was well established. But other severe infections could also associated with kidney disease.
- Exposure to cold, which was blamed for many cases of nephritis in adults that did not seem to have another explanation.
- ‘Renal irritants’ (toxins) such as turpentine, arsenic.
To a modern reader this mixes acute glomerulonephritis with many other pathologies, but these distinctions could only be beginning to be understood at the time. Microscopy was still crude. Although use of thin sections for microscopy was first described in 1839, staining and embedding came later. Studies could only be undertaken post-mortem.
It was a disease predominantly of the young, and the clinical course of most, particularly children, followed the typical pattern of post-Streptococcal disease: The symptom which commonly first attracts notice is oedema … the urine is darker, and in smaller quantity … there is probably pain in the loins. In its most acute form … urine becomes black with blood, and loaded with a dark sediment. … The pulse is hard and full (hypertension) … If the renal mischief be very intense, the urine may be reduced to 2 oz. or 3 oz. a day … This condition cannot last long. … The kidneys (at autopsy) will be gorged with blood, greatly increased in bulk … (Figure 2)
 |
| Figure 2. Section of a kidney in a state of acute Nephritis, the result of Scarlatina. (Dickinson 1877, Plate 1) |
Most patients did not die so early in the disease, but that was the usual outcome in adults: The dropsy will gain ground, involving the serous cavities, and death will take place in a month or six weeks, with coma preceded or not by epileptiform seizures (probably hypertensive). Or it may happen that he will be cut off by acute inflammation of the lungs (probably pulmonary oedema).
However many children recovered, and very occasional adults: If the disorder take a favourable turn, the urine would increase in quantity, the dropsy (generalised oedema) subside, and proteinuria at length would subside too. Infection of dropsical limbs, vomiting, nosebleeds, pericarditis and other symptoms were also noted.
If the course was prolonged, hypertrophy of the heart and hardness of the pulse were prominent. Many of these patients will have had other types of glomerulonephritis.
The case of a luckier 22 year old medical student is recounted second hand: He developed sudden haematuria without obvious preceding illness: Dr Barlow tested his urine and found upon the addition of nitric acid that it was literally converted into one clot of albumen. Dr Bright, who was consulted the next day, recommended the patient to leave town for the country, holding out no hope of recovery. The patient did leave for the country, with a daily urine output of 0.75 pints (less than 400ml) and with increasingly severe oedema; the urine was as dark as porter, and highly albuminous … the breath growing in tightness and difficulty. But he turned the corner after nearly a month of this, urine output increasing, swelling reducing, proteinuria coming down slowly and by two years undetectable. This was written up with 5 more examples in the Lancet in 1861, twenty years after the event, probably by the survivor himself, a Dr Williams of Swansea.
Dickinson also described late deterioration some years after an episode of apparently acute nephritis, patients by that late stage having contracted and granular kidneys.
Dickinson described many other cases in detail. The chapter on Treatment is a lesson in how limited the options were at that time. Scarlet fever remained an alarming illness – it was highly contagious and its complications, including nephritis, were potentially fatal.
In the 1920s vaccination against Streptococci was introduced, but it was general improvement in living standards, perhaps changing predominant micro-organisms, and Penicillin in the 1940s, that reduced the incidence so much that in the developed world post-Streptococal nephritis has become an uncommon condition.
Further reading
Dickinson WH (1867). Diseases of the Kidney and Urinary Derangements, Part 2 Albuminuria. Spottiswoode and Co., London. Available online
Williams T (1861). Recovery from Bright’s Disease. Lancet 78: 492-4.
Scarlet Fever (Wikipedia)