Alarming emergency and important public health marker
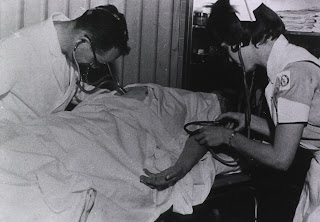 |
| Methodist Hospital, Dallas, 1966 (credit at foot of post) |
In the early days of dialysis obstetric renal failure was a major part of the work of a renal unit. Acute renal failure was estimated to occur in 1 in 1400 to 1 in 5000 pregnancies in the UK (in 2010 there were 13,400 births per million population in the UK, if you want to calculate how many referrals that would mean in your region). Over the next 20-30 years medical complications of pregnancy remained a regular and frightening reason for acute renal referrals. Frightening because patients are young and healthy till days before, with unfamiliar and rapidly changing physiology.
Hammersmith Hospital in West London had a special interest in acute renal failure from the 1940s, and attracted many referrals. In their 1965 report (Kinsey Smith et al) obstetric renal failure accounted for 15% of cases requiring dialysis between 1957 and 1965. However an estimate from Washington DC 10 years earlier (Schreiner and Berman 1955) was twice as high.
The 1965 London report came two years before the Abortion Act legalised abortion in England, Wales and Scotland. 40 of the 70 patients (Figure 2) presented in the first half of pregnancy, when most were associated with illegal abortion. These patients often presented late to hospital with sepsis or haemorrhage.
 |
| Fig 1 from Smith’s West London series 1965 (Lancet, with permission) |
The 30 patients who developed acute renal failure in late pregnancy mostly had variants of eclampsia/pre-eclampsia or obstetric haemorrhage. Eight failed to recover kidney function because of cortical necrosis, at this time a death sentence as long term dialysis and transplantation were not established.
The Hammersmith group had by this time moved from conservative treatment by strict management of fluid and dietary intake, through the use of haemodialysis, to routinely adopting peritoneal dialysis for the management of obstetric renal failure. The overall mortality was 35% with the late-onset group having worse outcomes. Obstetric and medical renal failure were regarded as lower-risk than surgical or traumatic renal failure.
Rates of obstetric renal failure have come down dramatically in the developed world, in line with falling maternal and infant mortality. So much so that renal trainees now see few cases. Abortion-associated renal failure is exceptionally rare. Early identification and management of pre-eclampsia have dramatically reduced the size of the late pregnancy group. Haemorrhage is more effectively managed and antibiotics have reduced the threat from infections. Much of obstetric-renal practice is now pregnancy in renal patients, rather than obstetric complications.
In other parts of the world many of these benefits of modern medicine and politics have yet to be felt. Obstetric renal failure remains a frightening part of acute nephrological practice in many developing countries. It is an indicator of levels of maternal morbidity and mortality, and influenced by the effective resource put into community-level healthcare and family planning. The profile of causes often closely resembles that described in London in 1965.
Further reading
Statistics on UK childbirth and mortality from the Royal College of Obstetricians and Gynaecologists (RCOG)
Gulshun Rehman. 2012. Malawi: reducing abortion-related deaths. Save the Children blog.
Smith K, JC McClure Browne, R Shackman, OM Wrong. 1965. Acute renal failure of obstetric origin. Lancet 286:351-4 (Pubmed)
Schreiner GE LB Berman. 1955. The clinical spectrum of postpartum acute renal insufficiency. Ann Intern Med 43:1230-40 (Pubmed)
Header image from US National Library of Medicine, Images of the History of Medicine.
One response to “Obstetric renal failure”
A Personal View in the British Medical Journal describes the distressingly common occurrence of renal failure and deaths from complications of abortion in Liberia today. http://www.bmj.com/content/345/bmj.e4391 (login required for the full article unfortunately)